Prostate cancer is the most common cancer in males in Scotland, with approximately 2,800 new cases diagnosed every year. Risk increases with age and approximately 99% of cases are diagnosed in men aged over 50 years. Men are 2.5 times more likely to be diagnosed with prostate cancer, if their father or brother has had it. In the UK, the lifetime risk of prostate cancer in Black men (1 in 4) is double that of the lifetime risk of all men combined (1 in 8).
Men presenting with unexplained possible symptoms and signs suggestive of prostate cancer such as changes to urinary patterns, erectile dysfunction, haematuria, lower back pain, bone pain or weight loss should have a digital rectal examination and a prostate specific antigen (PSA) test with counselling. A PSA test should not be performed within 1 month of a proven urinary tract infection (UTI). It should be noted that the majority of men with prostate cancer have no symptoms at all.
Visible haematuria is the most common presenting symptom for both bladder and kidney cancer. Other presenting features include loin pain, renal masses, non-visible haematuria, anaemia, weight loss and pyrexia. Both cancers are uncommon, with around 800 new bladder and 860 new kidney cancers each year.
Although scrotal swellings are a common presentation in general practice, testicular cancer is relatively rare, with around 200 new cases per annum, of which approximately 70% are between 15 and 45 years. Solid swellings affecting the body of the testis have a high probability (>50%) of being due to cancer. Cancer of the penis is rare, with around 60 new cases each year in Scotland, but its incidence is rising.
All patients presenting with symptoms or signs suggestive of urological cancer should be referred to a team specialising in the management of urological cancer, depending on local arrangements.
Prostate cancer
Evidence from digital rectal examination of a hard, irregular prostate
Elevated or rising age-specific PSA. Rough guide to normal PSA levels:
Bladder and kidney cancer
Testicular and penile cancer
Non urgent referral
Reference:
Scottish Referral Guidelines for Suspected Cancer. Scottish Government, August 2014
SIGN Guideline 85 – Management of transitional cell carcinoma of the bladder
Clinical Lead: Mr Rehan Khan, Consultant Urology Surgeon, NHS Lanarkshire
Review Date April 2017
| Renal Medicine | Consultant | Direct Line to Secretaries |
|---|---|---|
| Monklands Hospital | Dr W. G. J. Smith | 01236 712640 |
| Monkscourt Avenue | Dr M. F. Hand | 01236 712641 |
| Airdrie | Dr I. R. Shilliday | 01236 712582 |
| ML6 0JS | Dr J. P. Traynor | 01236 713167 |
| Switchboard | 01236 748748 | |
| Fax Number | 01236 712179 |
The renal unit is mostly centred at Monklands although we have some clinics at Wishaw and Hairmyres. It is likely that your patient will be reviewed at Monklands first. Background info on the renal unit is available via the FirstPort website. This also includes access to our guidelines including CKD guidelines and advice on the use of ACE inhibitors and ARBs. These are held in the Renal Documents Library on FirstPort
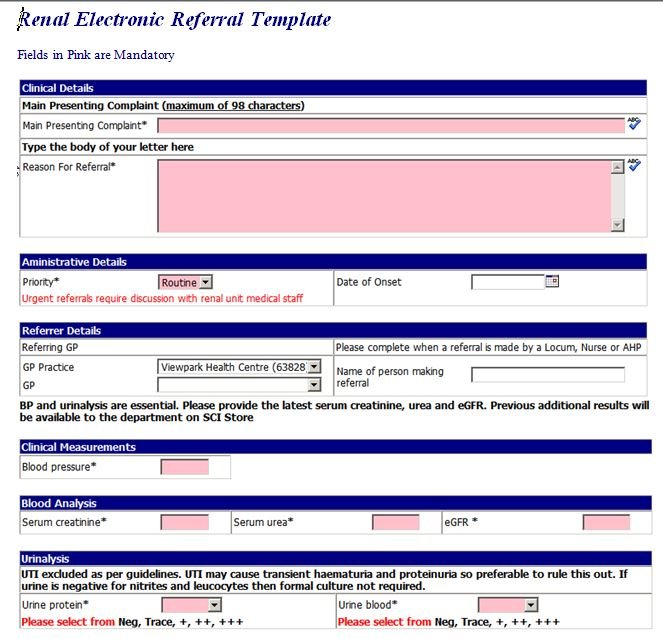
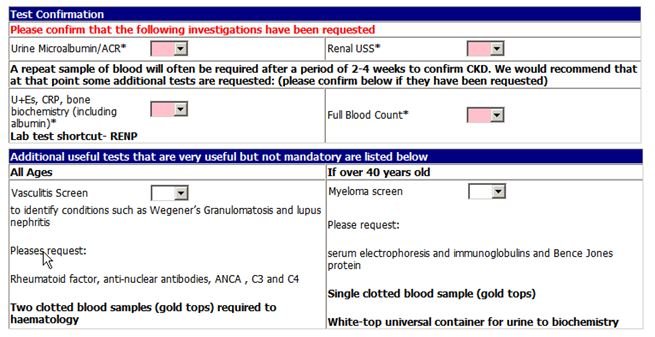
We have two categories of referral – routine and urgent. A routine patient will be seen in approximately 9 weeks. An urgent referral should be made if you think the patient may need to be admitted and we would prefer the urgent referral is coupled with a phone call at the time of referral to discuss the case.
For outpatient review (or at least discussion) include:
This will then trigger an USS which will include Renal size, renal cortex, aorta and presence or absence of hydronephrosis. If hydronephrosis is found, then a bladder USS will be undertaken.
If a renal mass is found, radiology will automatically self refer for CT and access the lab browsers for the eGFR (blood for this should have been taken as part of the renal referral process). Information regarding diabetes and metformin use should be included in the referral
The initial report will be sent to primary care as if there is a mass or obstruction this should be referred through to Urology. Renal team will have direct access to the reports in clinic so do not need the reports forwarded. With a clinic waiting time of 6-8 weeks, the USS will always be done before the patient is seen in clinic
On the main referral page several items are coded as mandatory fields. We hope you will be willing to put up with the minor frustration this might cause you to ensure that our mutual patient’s journey through the clinic system is made as meaningful and quick as possible.