People over the age of 65 with a psychological/emotional/severe or enduring mental health problem, including dementia.
High priority/urgent referrals should be followed up by a phone call to the relevant locality team to discuss degree of urgency, timescale for appointment etc.
A standard physical examination guided by symptoms +/- : BP, MSSU if indicated by history, CXRay if indicated by history, ECG if indicated by history etc.
Neuro-imaging is NOT expected/required to be ordered prior to referral.
NICE/RCPsych guidance on blood tests recommends full blood count, ESR or C-reactive protein (CRP), vitamin B12, folate, thyroid function, urea and electrolyte, calcium, liver function and glucose tests, with blood tests for syphilis, lipids and HIV listed as ‘optional’. (Royal College of Psychiatrists, 2005b).
The following is a description of tiered services within mental health to guide decision making and appropriate referral and signposting. In this context a tier refers to a service requirement with appropriate training and skills for delivery of patient care and is based on patient need, increasing complexity and risk assessments. It is based on the premise that patients will need to access a variety of health services dependent on their need throughout their lives, from those at primary care to those that are more specialised, and that a strategic approach to identify needs will best inform delivery of services and support evidenced based care.
Although it is anticipated the majority of GP colleagues will deal with Tier 1, Tier 2, Tier 3 and that they will treat and manage the majority of mental health problems in primary care, it is important to have information as to how best to use the services, to understand the range of treatments and interventions available and the need to ensure there are appropriate links with primary care as regards decision making at secondary care. Although GP colleagues may have less contact with Tier 4 their role will also be important in terms of sharing information and guiding secondary care on primary care interventions and treatments as part of multidisciplinary risk assessments and planning of care.
For the sake of completion Tier 0 refers to community, public health and strategic approaches to promote the general health and well being of patients and is not included here.
Currently and to allow the service to further develop we have combined the existing structures within psychology and how it would link with psychiatry services for the purposes of facilitating a referral system that is seamless from primary to secondary care , this will be reviewed and may be subject to further revision as services further evolve.
In Tier 4 highly specialist services provide aspects of Mental Health Care (mainly Forensic and Rehabilitation services) that may not be able to be provided within community secondary care services (of Tier 2 and 3). Currently there is no direct referral into this service from primary care but future developments of service may consider this.
CMHTs (Community Mental Health Teams) are at the heart of secondary care services in Tier 3 and provide services to patients aged 16-65 and who have left school.
Patients aged 16-18 years who are still at school are the remit of Child and adolescent mental health services.
CMHTS also provide an emergency response to patients who are suffering a mental health crisis and require to be seen the same day, consequently each CMHT has a duty worker system and referrals can be taken 08:30-18:30 Monday to Friday and at weekends 10:00-16:30.
General guidance as to patients who would benefit from the Service includes:
Assessment/treatment of mild to moderate common mental health problems (including Specific Phobias, Panic Disorder, Generalised Anxiety Disorder, Social Phobias, Health Anxiety, complicated or prolonged grief reactions, psycho-sexual difficulties, Habit Disorders and includes mild and moderate depression.
For the purposes of clarity as regards the definition of depression it includes the following:
(A) Community Support Options:
(B) Specialist Mental Health Support:
The identification, assessment and treatment of mild common mental health problems, such as anxiety and depression.
Although it is recognised that the majority of patients with mental health problems are treated in primary care, and effective treatment is available. As part of ongoing work in NHSL to standardise treatments it is important that patients are offered choices for treatment that follow evidence based guidelines.
As a consequence, it is expected that as part of the GPs repertoire of choices for patients, it is assumed that there has been an attempt to offer and inform the patient of self help, telephone help lines, website based CBT and NHS 24 CBT, or specific counselling including:
CRUSE for bereavement – www.cruse.org.uk
RELATE for marriage or relationship difficulties – www.relate.org.uk
PETAL for patients experiencing trauma and loss after a murder or suicide – www.petalsupport.com
and that the patients have been unable to or it has not been possible to engage with these interventions before referral to the secondary care services.
Pre treatment presentations will include the identification, assessment and treatment of mild common mental health problems, such as anxiety and depression. For patients who have been unable to access or unable to engage with common interventions that include:
A Helpful guide includes SIGN Guideline 114 for depression that concentrates on the non pharmaceutical management of depression. SIGN 114 Download
The following is a description of tiered services within mental health to guide decision making and appropriate referral and signposting. In this context a tier refers to a service requirement with appropriate training and skills for delivery of patient care and is based on patient need, increasing complexity and risk assessments. It is based on the premise that patients will need to access a variety of health services dependent on their need throughout their lives, from those at primary care to those that are more specialised, and that a strategic approach to identify needs will best inform delivery of services and support evidenced based care.
Although it is anticipated the majority of GP colleagues will deal with Tier 1, Tier 2, Tier 3 and that they will treat and manage the majority of mental health problems in primary care, it is important to have information as to how best to use the services, to understand the range of treatments and interventions available and the need to ensure there are appropriate links with primary care as regards decision making at secondary care. Although GP colleagues may have less contact with Tier 4 their role will also be important in terms of sharing information and guiding secondary care on primary care interventions and treatments as part of multidisciplinary risk assessments and planning of care.
For the sake of completion Tier 0 refers to community, public health and strategic approaches to promote the general health and well being of patients and is not included here.
Currently and to allow the service to further develop we have combined the existing structures within psychology and how it would link with psychiatry services for the purposes of facilitating a referral system that is seamless from primary to secondary care , this will be reviewed and may be subject to further revision as services further evolve.
In Tier 4 highly specialist services provide aspects of Mental Health Care (mainly Forensic and Rehabilitation services) that may not be able to be provided within community secondary care services (of Tier 2 and 3). Currently there is no direct referral into this service from primary care but future developments of service may consider this.
CMHTs (Community Mental Health Teams) are at the heart of secondary care services in Tier 3 and provide services to patients aged 16-65 and who have left school.
Patients aged 16-18 years who are still at school are the remit of Child and adolescent mental health services.
CMHTS also provide an emergency response to patients who are suffering a mental health crisis and require to be seen the same day, consequently each CMHT has a duty worker system and referrals can be taken 08:30-18:30 Monday to Friday and at weekends 10:00-16:30.
General guidance as to patients who would benefit from the Service includes:
Assessment/treatment of mild to moderate common mental health problems (including Specific Phobias, Panic Disorder, Generalised Anxiety Disorder, Social Phobias, Health Anxiety, complicated or prolonged grief reactions, psycho-sexual difficulties, Habit Disorders and includes mild and moderate depression.
For the purposes of clarity as regards the definition of depression it includes the following:
(A) Community Support Options:
(B) Specialist Mental Health Support:
The identification, assessment and treatment of mild common mental health problems, such as anxiety and depression.
Although it is recognised that the majority of patients with mental health problems are treated in primary care, and effective treatment is available. As part of ongoing work in NHSL to standardise treatments it is important that patients are offered choices for treatment that follow evidence based guidelines.
As a consequence, it is expected that as part of the GPs repertoire of choices for patients, it is assumed that there has been an attempt to offer and inform the patient of self help, telephone help lines, website based CBT and NHS 24 CBT, or specific counselling including:
CRUSE for bereavement – www.cruse.org.uk
RELATE for marriage or relationship difficulties – www.relate.org.uk
PETAL for patients experiencing trauma and loss after a murder or suicide – www.petalsupport.com
and that the patients have been unable to or it has not been possible to engage with these interventions before referral to the secondary care services.
Pre treatment presentations will include the identification, assessment and treatment of mild common mental health problems, such as anxiety and depression. For patients who have been unable to access or unable to engage with common interventions that include:
A Helpful guide includes SIGN Guideline 114 for depression, that concentrates on the non pharmaceutical management of depression.
The following is a description of tiered services within mental health to guide decision making and appropriate referral and signposting. In this context a tier refers to a service requirement with appropriate training and skills for delivery of patient care and is based on patient need, increasing complexity and risk assessments. It is based on the premise that patients will need to access a variety of health services dependent on their need throughout their lives, from those at primary care to those that are more specialised, and that a strategic approach to identify needs will best inform delivery of services and support evidenced based care.
Although it is anticipated the majority of GP colleagues will deal with Tier 1, Tier 2, Tier 3 and that they will treat and manage the majority of mental health problems in primary care, it is important to have information as to how best to use the services, to understand the range of treatments and interventions available and the need to ensure there are appropriate links with primary care as regards decision making at secondary care. Although GP colleagues may have less contact with Tier 4 their role will also be important in terms of sharing information and guiding secondary care on primary care interventions and treatments as part of multidisciplinary risk assessments and planning of care.
For the sake of completion Tier 0 refers to community, public health and strategic approaches to promote the general health and well being of patients and is not included here.
Currently and to allow the service to further develop we have combined the existing structures within psychology and how it would link with psychiatry services for the purposes of facilitating a referral system that is seamless from primary to secondary care, this will be reviewed and may be subject to further revision as services further evolve.
In Tier 4 highly specialist services provide aspects of Mental Health Care (mainly Forensic and Rehabilitation services) that may not be able to be provided within community secondary care services (of Tier 2 and 3). Currently there is no direct referral into this service from primary care but future developments of service may consider this.
CMHTs (Community Mental Health Teams) are at the heart of secondary care services in Tier 3 and provide services to patients aged 16 – 65 and who have left school.
Patients aged 16-18 years who are still at school are the remit of Child and adolescent mental health services.
CMHTS also provide an emergency response to patients who are suffering a mental health crisis and require to be seen the same day, consequently each CMHT has a duty worker system and referrals can be taken 08:30 – 18:30 Monday to Friday and at weekends 10:00 – 16:30.
General guidance as to patients who would benefit from the Service includes:
Assessment/treatment of mild to moderate common mental health problems (including Specific Phobias, Panic Disorder, Generalised Anxiety Disorder, Social Phobias, Health Anxiety, complicated or prolonged grief reactions, psycho-sexual difficulties, Habit Disorders and includes mild and moderate depression.
For the purposes of clarity as regards the definition of depression it includes the following:
(A) Community Support Options:
(B) Specialist Mental Health Support:
(C) Beating The Blues
Beating The Blues has a specific referral protocol which is available in the Mental Health Lanarkshire Wide Services branch of SCI Gateway.
Referral Criteria for Beating the Blues:
The identification, assessment and treatment of mild common mental health problems, such as anxiety and depression.
Although it is recognised that the majority of patients with mental health problems are treated in primary care, and effective treatment is available. As part of ongoing work in NHSL to standardise treatments it is important that patients are offered choices for treatment that follow evidence based guidelines.
As a consequence, it is expected that as part of the GPs repertoire of choices for patients, it is assumed that there has been an attempt to offer and inform the patient of self help, telephone help lines, website based CBT and NHS 24 CBT, or specific counselling including:
CRUSE for bereavement – www.cruse.org.uk
RELATE for marriage or relationship difficulties – www.relate.org.uk
PETAL for patients experiencing trauma and loss after a murder or suicide – www.petalsupport.com
and that the patients have been unable to or it has not been possible to engage with these interventions before referral to the secondary care services.
Pre treatment presentations will include the identification, assessment and treatment of mild common mental health problems, such as anxiety and depression. For patients who have been unable to access or unable to engage with common interventions that include:
A Helpful guide includes SIGN Guideline 114 for depression that concentrates on the non pharmaceutical management of depression SIGN 114 Download
Reference:
Lead Clinician: Michael Ross, Head of Adult Psychological Services
Review Date September 2016
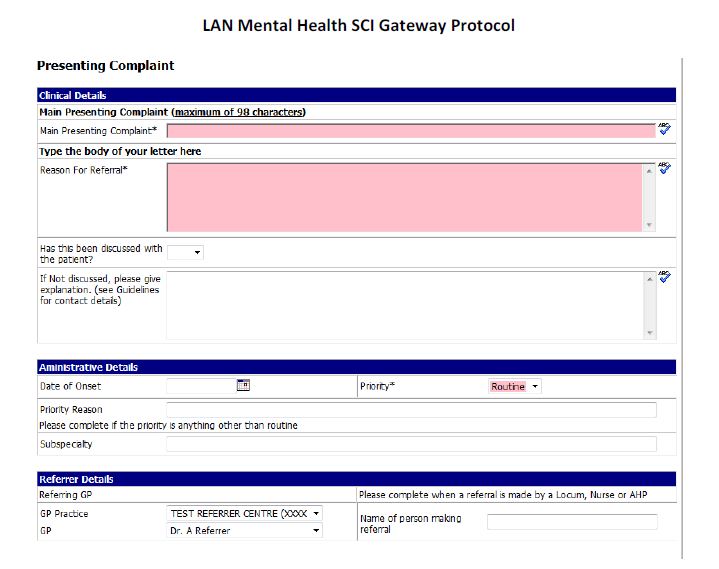
This is a dictation template to provide a reminder of the information required to complete the referral. The fields in red are mandatory and must be completed on the referral protocol.
Main Presenting Complaint: [Beating the Blues Referral]
Has this been discussed with the patient:
If not discussed, please give explanation. (See Guidelines for contact details): [Text]
Date of Onset: [Date]
Priority: [Routine]
Is the patient currently taking anti-depressants:
Please indicate the persons education level:
Preferred method of communication:
Please provide details if not complete:
Mobile phone number: [Text]
Email Address: [Text]
Criteria for Referral to Tier 3 Services
Dependency
Pharmacological
Psychiatry /Psychology
Physical Health Damaged
Alcohol Related Brain Damage
Complex Social / Health Needs
Access to rehabilitation / residential in Patient Interventions
Criteria for Referral to Tier 2 Services
Early Intervention
Harmful / Hazardous Drinking
Drinking Drugs Precipitated by Major Life Events
Counselling / Support Work for Individuals and Families
Family Counselling / Mediation
Non-medical Interventions
Education / Prevention / Information/Advice
North Lanarkshire: Definitions for Tier 3: Referral to North Lanarkshire Integrated Service
| Dependency | Using alcohol/drugs daily : unable to function without use or consumption | |
|---|---|---|
| 1 | Pharmacological Needs | Detoxification / substitute prescribing / Antabuse / Disulfiram |
| 2 | Psychiatric Issues | Requires specialist Psychiatric Input |
| 3 | Physical Health | Any Addiction Related Health Problem |
| 4 | Access to Rehabilitation / Residential Inpatient | Acute mental health care, requiring comprehensive assessment and funding to be identified |
| 5 | Alcohol Related Brain Damage | Changes to the structure and function of the brain resulting from long term consumption of alcohol |
| 6 | Psychology | Requires specialist Psychological Input, Psychosocial Interventions |
| 7 | ASP Adults who have addiction issues which could meet the criteria for Adult Support and Protection | “Adults at risk” are adults who:- Are unable to safeguard their own wellbeing, property, rights and other interests Are at risk of harm Because they are affected by disability, mental disorder, illness or physical or mental infirmity, are more vulnerable to being harmed than an adult who are so affected |
| 8 | Child Protection | Issues where children may be offered by parental substance misuse |
| 9 | Complex Social Needs | Homeless / Criminal Justice Involvement / Multi Agency Involvement |
| 10 | Community Care Needs | Complex needs requiring specialist input: health; family; relationships; problems in taking care of themselves; not coping with everyday events; multiple problems |
North Lanarkshire: Common Definitions for Tier 2 Service
| Early Intervention: | Pre - Dependency | |
|---|---|---|
| 1 | Non-medical interventions | Counselling / Support Work / Group work / Telephone Support |
| 2 | Harmful / Hazardous Drinking | Hazardous drinking above safer drinking limits. The person has so far avoided significant alcohol-related problems. Harmful - is drinking above safe levels with evidence of alcohol-related problems. May show a mild level of dependence |
| 3 | Experiential / Recreational drug use: | A drug used non-medically for personal enjoyment. Usually used in affecting mental activity, behaviour, or perception, as a mood-altering drug. |
| 4 | Drinking / Drugs Precipitated by Major Life Events: | Individuals using alcohol/drugs to cope with major events, e.g., death, divorce, financial hardship; unemployment |
| 5 | Counselling / Support Work for Individuals | Counselling involves one person (the counsellor) helping another person (the client) to work through some difficult or painful emotional, behavioural or relationship problem or difficulty |
| 6 | Counselling / Support Work for significant others / families: | Support for significant others who are concerned about a loved one’s drink or drug use. The support enables the significant other to be heard and feel more able to understand and cope with the situation |
| 7 | ASP Family Counselling / Mediation | Family counselling / mediation can help reduce conflict which means fewer rows at home and can help everyone cope better with their situation. |
| 8 | Education / Prevention | Group work / Information leaflets |
| 9 | Information/Advice | Up to date information e.g. Alcohol Unit calculation, Alcohol / Drug effects on the body |
South Lanarkshire: Common Definitions for Tier 2:
| Early Intervention: | Pre - Dependency | |
|---|---|---|
| 1 | Non-medical interventions | Counselling / Support Work / Group work / Telephone Support |
| 2 | Harmful / Hazardous Drinking | Hazardous - drinking above safer drinking limits. The person has so far avoided significant alcohol-related problems. Harmful - is drinking above safe levels with evidence of alcohol-related problems. May show a mild level of dependence |
| 3 | Experiential/recreational drug use: | A drug used non-medically for personal enjoyment. Usually used in affecting mental activity, behaviour, or perception, as a mood-altering drug. |
| 4 | Drinking / Drugs Precipitated by Major Life Events: | Individuals using alcohol/drugs to cope with major events, e.g., death, divorce, financial hardship; unemployment |
| 5 | Counselling / Support Work for Individuals | Counselling involves one person (the counsellor) helping another person (the client) to work through some difficult or painful emotional, behavioural or relationship problem or difficulty |
| 6 | Counselling / Support Work for significant others / families: | Support for significant others who are concerned about a loved one’s drink or drug use. The support enables the significant other to be heard and feel more able to understand and cope with the situation |
| 7 | Family Counselling / Mediation | Family counselling/ mediation can help reduce conflict which means fewer rows at home and can help everyone cope better with their situation. |
| 8 | Education / Prevention | Group work / information leaflets Relapse Prevention / Alcohol Brief Intervention |
| 9 | Information / Advice | Up to date information e.g. Alcohol Unit calculation Alcohol/Drug effects on the body |
South Lanarkshire: Definitions for Tier 3: Referral to LAADS or SMT
| Dependency | Using alcohol/drugs daily : unable to function without use or consumption | Refer to | |
|---|---|---|---|
| 1 | Pharmacological Needs | Detoxification / Substitute prescribing / Antabuse / Disulfiram | LAADS |
| 2 | Psychiatric Issues | Requires specialist Psychiatric Input | LAADS |
| 3 | Physical Health | Any Addiction Related Health Problem | LAADS |
| 4 | Access to Rehabilitation / Residential In-Patient | Acute mental health care, requiring comprehensive assessment and funding to be identified | LAADS / SMT |
| 5 | Alcohol Related Brain Damage: | Changes to the structure and function of the brain resulting from long term consumption of alcohol. | LAADS / SMT |
| 6 | Psychosocial Interventions | Requires specialist Psychological Input | LAADS / SMT |
| 7 | ASP Adults who have addiction issues which could meet the criteria for Adult Support and Protection. | "Adults at risk” are adults who:- Are unable to safeguard their own wellbeing, property, rights and other interests Are at risk of harm Because they are affected by disability, mental disorder, illness or physical or mental infirmity, are more vulnerable to being harmed than an adult who are so affected. | |
| 8 | Child Protection | SMT | |
| 9 | Complex Social Needs | Homeless / Criminal Justice Involvement / Multi Agency Involvement | SMT |
| 10 | Community Care Needs | Complex needs requiring specialist input: health; family; relationships; problems in taking care of themselves; not coping with everyday events; multiple problems | SMT |
South Lanarkshire
| Teir 3 | Health | LAADS |
| Teir 3 | Social | SMT |
| Teir 2 | Non Medical | Meridian |